Connect With Us

Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.
Why Live with Pain and Numbness in Your Feet?
Custom Orthotics Provide Relief From Heel Pain
Experiencing persistent heel pain? Custom Orthotics might be your solution. These custom-designed shoe inserts adapt to your unique foot structure, optimizing support and alleviating discomfort. By redistributing pressure, they can significantly reduce heel pain, enhancing your daily mobility. Dive into a pain-free lifestyle and elevate your walking experience. Curious about the benefits of Custom Orthotics?
Contact our office today.
Key Facts About Poor Foot Circulation

Poor foot circulation is a condition where blood flow to the feet is reduced, leading to various health issues. It often results in symptoms such as cold feet, numbness, and swelling. Common causes include diabetes, peripheral artery disease, and prolonged inactivity. Smoking and high cholesterol levels can also contribute to this condition. Poor circulation can delay healing of wounds and increase the risk of infections due to inadequate blood supply. Regular exercise, such as walking or stretching, can improve circulation by stimulating blood flow. Wearing compression socks can also help manage symptoms by promoting venous return. Maintaining a healthy diet and managing underlying conditions is essential for preventing poor foot circulation. Having poor foot circulation can be uncomfortable, and the causes often need to be identified before starting treatment. If you have poor foot circulation, it is suggested that you consult with a podiatrist who can properly diagnose this condition and offer appropriate relief solutions.
Poor circulation is a serious condition and needs immediate medical attention. If you have any concerns with poor circulation in your feet contact one of our podiatrists of Fox Valley Foot and Ankle Specialists. Our doctors will treat your foot and ankle needs.
Poor Circulation in the Feet
Poor blood circulation in the feet and legs is can be caused by peripheral artery disease (PAD), which is the result of a buildup of plaque in the arteries.
Plaque buildup or atherosclerosis results from excess calcium and cholesterol in the bloodstream. This can restrict the amount of blood which can flow through the arteries. Poor blood circulation in the feet and legs are sometimes caused by inflammation in the blood vessels, known as vasculitis.
Causes
Lack of oxygen and oxygen from poor blood circulation restricts muscle growth and development. It can also cause:
- Muscle pain, stiffness, or weakness
- Numbness or cramping in the legs
- Skin discoloration
- Slower nail & hair growth
- Erectile dysfunction
Those who have diabetes or smoke are at greatest risk for poor circulation, as are those who are over 50. If you have poor circulation in the feet and legs it may be caused by PAD and is important to make changes to your lifestyle in order to reduce risk of getting a heart attack or stroke. Exercise and maintaining a healthy lifestyle will dramatically improve conditions.
As always, see a podiatrist as he or she will assist in finding a regimen that suits you. A podiatrist can also prescribe you any needed medication.
If you have any questions please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes Symptoms and Treatment for Poor Circulation in the Feet
The purpose of the body’s circulation system is to transport blood, oxygen, and nutrients throughout the body. A reduction of blood to a specific part of the body may cause one to experience symptoms of poor circulation. The most common causes of poor circulation in the feet are obesity, diabetes, and heart conditions such as peripheral artery disease (PAD). Common symptoms of poor circulation include tingling, numbness, throbbing, pain and muscle cramps.
Peripheral artery disease is a common cause of poor circulation in the legs. Symptoms of PAD are cramping, pain or tiredness in the leg or hip muscles while walking or climbing stairs. This pain tends to go away with rest and starts back up when you begin to walk. It is a condition that causes the blood vessels and arteries to become narrow. Although PAD is more common in adults over the age of 50, it may also occur in younger people. A similar condition called atherosclerosis causes arteries to stiffen up due to a buildup of plaque in the arteries and blood vessels.
Blood clots are also a common cause of poor circulation in the feet. Clots may obstruct blood vessels and if they occur in the legs, they may eventually lead to pain and discoloration. This occurrence is commonly known as deep vein thrombosis (DVT) and it may travel to the lungs. Varicose veins are another condition that may lead to poor circulation, and it is caused by incompetence of the valves in the veins. Women who are overweight are prone to developing this condition. Lastly, diabetes, which is correlated with poor blood sugar metabolism may lead to chronic poor circulation. Those with diabetes often suffer from cramping in the legs, calves, thighs and buttocks.
If you are looking for ways to avoid poor circulation there are some tips you can follow. One tip is to avoid sitting for too long. If you plan to sit down for a long period of time, you should try standing up occasionally, to improve your circulation. Another great way to avoid poor circulation is to exercise. Exercise is an excellent way to pump the heart and increase blood flow. Those who suffer from poor circulation should also avoid smoking, reduce their salt intake, and try to lose weight.
If you are experiencing symptoms from poor circulation in your feet, you should consult with your podiatrist to determine the best method for treatment for you. He or she may prescribe medication in addition to recommending specific lifestyle changes to improve your circulation.
Orthotics Can Target Various Foot Conditions

Foot orthotics, also known as orthotic insoles or shoe inserts, are custom-designed devices that are placed inside shoes to support and align the feet properly. These inserts serve a variety of purposes, addressing a range of foot conditions such as flat feet, plantar fasciitis, bunions, and arthritis. By providing cushioning, stability, and corrective support, orthotics help alleviate pain, improve foot function, and prevent further complications. A podiatrist, specializing in the diagnosis and treatment of foot disorders, plays a vital role in identifying and addressing foot problems. Through a comprehensive examination, which may include a physical assessment, imaging tests, and gait analysis, podiatrists can accurately diagnose conditions affecting the feet and ankles. With their expertise and knowledge of biomechanics, podiatrists can recommend appropriate orthotic interventions tailored to each patient's specific needs. If you have a foot condition that can benefit from wearing custom-made orthotics, it is suggested that you are under the care of a podiatrist who can determine if this is the correct decision for you.
If you are experiencing discomfort in your feet and would like to try custom orthotics, contact one of our podiatrists from Fox Valley Foot and Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Are Custom Orthotics?
Custom orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain.
Over-the-Counter Inserts
Shoe inserts come in a wide variety and are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality, custom inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you're experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibility of using custom orthotics or shoe inserts. A podiatrist can determine which type of custom orthotic or shoe insert is right for you and help you take the first steps toward being pain-free.
If you have any questions please contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Investing in Custom Orthotics Means Investing in Foot Health
Custom orthotics offer a tailored approach to foot health, providing a host of benefits that extend far beyond conventional shoe inserts. One of the primary advantages lies in their ability to address specific biomechanical issues. Unlike off-the-shelf inserts, custom orthotics are crafted based on an individual's unique foot structure, gait, and any existing foot conditions.
The personalized design of custom orthotics ensures optimal support for the arches, promoting proper alignment and distributing pressure evenly across the feet. This can be particularly beneficial for individuals dealing with issues such as overpronation or underpronation, as custom orthotics help correct imbalances that may lead to discomfort or injury.
Beyond biomechanics, custom orthotics can alleviate a range of foot problems, including plantar fasciitis, bunions, and metatarsalgia. They provide targeted relief to areas under stress, reducing pain and inflammation. Additionally, for those with specific medical conditions like diabetes, custom orthotics can play a crucial role in preventing complications associated with poor foot health.
Comfort is another key aspect of custom orthotics. By accommodating the unique contours of an individual's feet, these inserts enhance overall comfort, making daily activities more enjoyable. Whether for athletes looking to optimize performance or individuals seeking relief from chronic foot pain, custom orthotics offer a versatile solution.
Investing in custom orthotics is an investment in long-term foot health. They not only provide immediate relief but also contribute to the prevention of future issues. With the ability to seamlessly integrate into various types of footwear, custom orthotics empower individuals to prioritize foot comfort without compromising on style. In essence, custom orthotics are a personalized prescription for happy, healthy, and pain-free feet.
Life Quality With Heel Pain
 Plantar fasciitis significantly impacts quality of life, primarily due to persistent heel pain. This condition involves inflammation of the plantar fascia, a thick band of tissue running along the bottom of the foot, often resulting in stabbing pain, particularly during the first steps in the morning or after periods of inactivity. The pain can range from a dull ache to sharp discomfort, making walking, standing, and engaging in daily activities challenging. Symptoms can include heel pain, stiffness, and swelling. Common causes are overuse, wearing improper footwear, obesity, and excessive standing or walking on hard surfaces. Relief options include rest, stretching exercises, proper footwear, and orthotic devices to provide arch support. In severe cases, medical interventions such as corticosteroid injections or surgery might be necessary. If you suffer from plantar fasciitis, it is suggested that you schedule an appointment with a podiatrist to manage it and prevent further complications.
Plantar fasciitis significantly impacts quality of life, primarily due to persistent heel pain. This condition involves inflammation of the plantar fascia, a thick band of tissue running along the bottom of the foot, often resulting in stabbing pain, particularly during the first steps in the morning or after periods of inactivity. The pain can range from a dull ache to sharp discomfort, making walking, standing, and engaging in daily activities challenging. Symptoms can include heel pain, stiffness, and swelling. Common causes are overuse, wearing improper footwear, obesity, and excessive standing or walking on hard surfaces. Relief options include rest, stretching exercises, proper footwear, and orthotic devices to provide arch support. In severe cases, medical interventions such as corticosteroid injections or surgery might be necessary. If you suffer from plantar fasciitis, it is suggested that you schedule an appointment with a podiatrist to manage it and prevent further complications.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Fox Valley Foot and Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is the thick band of tissue that connects the heel bone to the toes. When this band of connective tissue becomes inflamed, plantar fasciitis occurs. Fortunately, this condition is treatable.
There are several factors that may put you at a greater risk for developing plantar fasciitis. One of the biggest factors is age; plantar fasciitis is common in those between the ages of 40 to 60. People who have jobs that require them to be on their feet are also likely to develop plantar fasciitis. This includes factory workers, teachers, and others who spend a large portion of their day walking around on hard surfaces. Another risk factor is obesity because excess weight can result in extra stress being placed on the plantar fascia.
People with plantar fasciitis often experience a stabbing pain in the heel area. This pain is usually at its worst in the morning, but can also be triggered by periods of standing or sitting. Plantar fasciitis may make it hard to run and walk. It may also make the foot feel stiff and sensitive, which consequently makes walking barefoot difficult.
Treatment for plantar fasciitis depends on the severity of the specific case of the condition. Ice massage applications may be used to reduce pain and inflammation. Physical therapy is often used to treat plantar fasciitis, and this may include stretching exercises. Another treatment option is anti-inflammatory medication, such as ibuprofen.
If you suspect that you have plantar fasciitis, meet with your podiatrist immediately. If left untreated, symptoms may lead to tearing and overstretching of the plantar fascia. The solution is early detection and treatment. Be sure to speak with your podiatrist if you are experiencing heel pain.
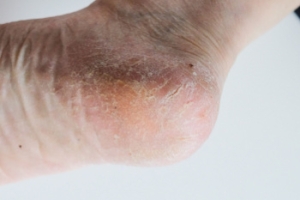
Cracked Heels Can Be Unsightly and Painful
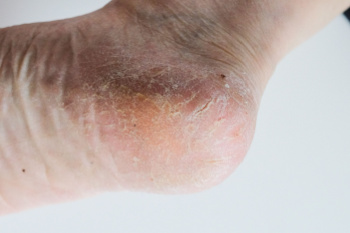 Cracked heels occur when the skin on the heels becomes dry and thickens, leading to fissures. The cracks can be caused by prolonged standing, wearing open-back shoes, and skin conditions such as eczema or psoriasis. Cracked heels often appear as dry, rough patches with visible splits, which can feel painful and tender, especially when pressure is applied. Beyond their unsightly appearance, cracked heels can lead to serious complications. The deep fissures can become infected, causing swelling, redness, and bleeding. If left untreated, this can result in cellulitis, a painful bacterial skin infection. For individuals with diabetes or compromised immune systems, the risks are even greater because infections can spread easily and become severe. To prevent and treat cracked heels, it is suggested that you schedule an appointment with a podiatrist who can provide effective treatment solutions, and prevent further complications.
Cracked heels occur when the skin on the heels becomes dry and thickens, leading to fissures. The cracks can be caused by prolonged standing, wearing open-back shoes, and skin conditions such as eczema or psoriasis. Cracked heels often appear as dry, rough patches with visible splits, which can feel painful and tender, especially when pressure is applied. Beyond their unsightly appearance, cracked heels can lead to serious complications. The deep fissures can become infected, causing swelling, redness, and bleeding. If left untreated, this can result in cellulitis, a painful bacterial skin infection. For individuals with diabetes or compromised immune systems, the risks are even greater because infections can spread easily and become severe. To prevent and treat cracked heels, it is suggested that you schedule an appointment with a podiatrist who can provide effective treatment solutions, and prevent further complications.
If the skin on your feet starts to crack, you may want to see a podiatrist to find treatment. If you have any concerns, contact one of our podiatrists from Fox Valley Foot and Ankle Specialists. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
It is important to moisturize your cracked heels in order to prevent pain, bleeding, and infection. The reason cracked heels form is because the skin on the foot is too dry to support the immense pressure placed on them. When the foot expands, the dry skin on the foot begins to split.
Ways to Help Heal Them
- Invest in a good foot cream
- Try Using Petroleum Jelly
- Ease up on Soaps
- Drink Plenty of Water
Ways to Prevent Cracked Heels
- Moisturize After Showering
- Skip a Shower
- Keep Shower Water Lukewarm
- Don’t Scrub Your Feet
If you are unsure how to proceed in treating cracked heels, seek guidance from a podiatrist. Your doctor will help you with any questions or information you may need.
If you have any questions, please feel free to contact our office located in Naperville, IL . We offer the newest diagnostic and treatment technologies for all your foot care needs.